Home » Tuberous Breast Correction Surgery: How It Works and

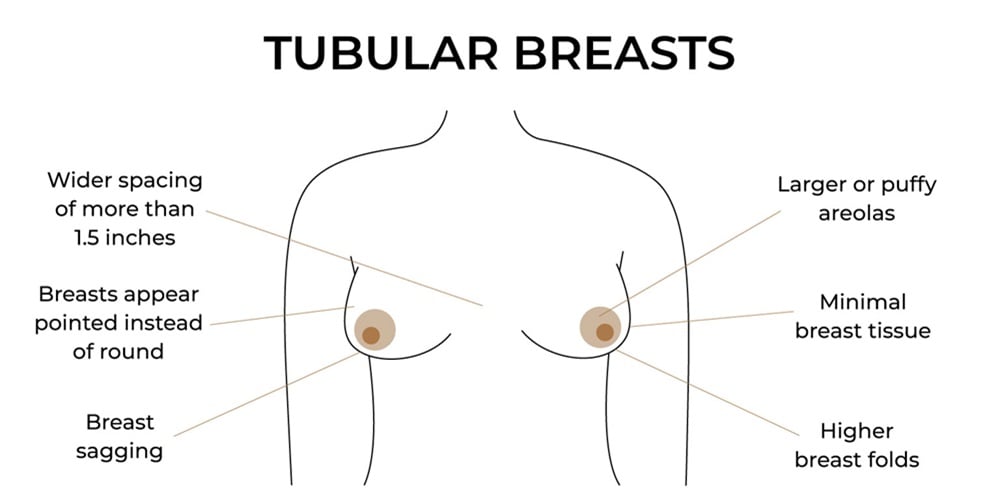
Tuberous breast deformity is a term that has been used to describe a whole range of breast shapes, which are breast aesthetics that some might consider not normal. The hallmarks of a tuberous breast repair are building out the lower pole and correcting the herniation of the areola by reducing the constricted and tight tissue that has held the breast back. Curable with surgery, tuberous breast correction is both about improving the appearance and worth of the patient’s body. Restoring a natural, relaxed shape to all structures is what needs to be achieved in tuberous breast reconstruction; the goal is not to simply reduce the space from the chest wall to the nipple to get a bigger, normal silhouette. There are many different beliefs about when and why some women develop tuberous breasts. The clear fact is that tuberous breast repair can happen from birth or during a child’s growing years. What is obvious is that it may not directly be the patient’s fault that they are dealing with these issues. The emotional toll and feelings of physical insecurity that often connect to the abnormal birth shape make up the psychological side of tuberous breast deformity. The men and women who enjoy long-lasting results that look as well as feel natural are those who have improved their bodies with tuberous breast repair. Understanding what a tuberous breast correction looks like is a crucial first step towards potentially getting one. Though not every patient will display every sign, constricted or tuberous breasts often feature some common physical and emotional attributes. Most tuberous breasts show extra-lateral space between them and the softer breast mounds.
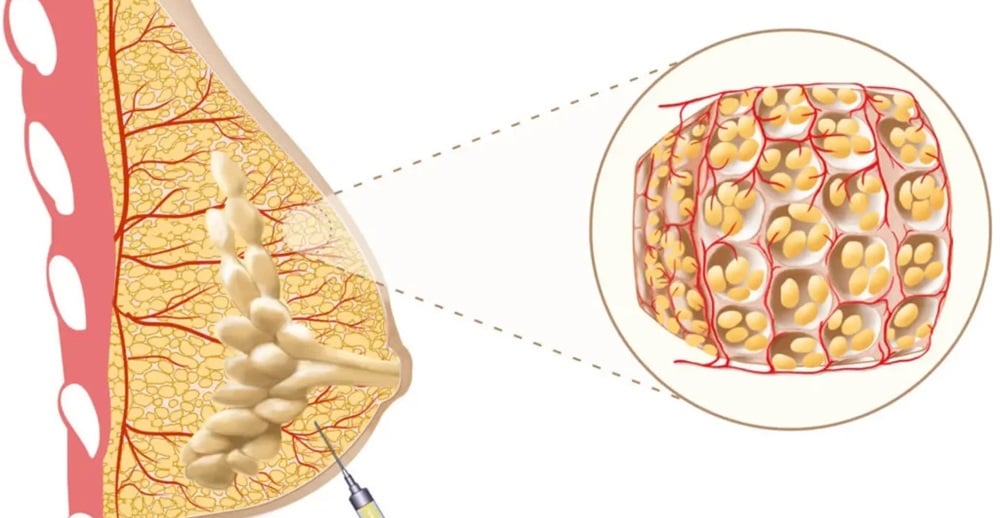
Liposuction: Many tuberous women have a form of adipose tissue constriction that can be treated with liposuction to free the base of the breast and create a more natural shape. Large, long accessory breasts might be good candidates for simple liposuction fat reduction. Breast Augmentation: One or two-stage tissue expansion to stretch the hard ring constrictions of the breast to create a new normal soft-bra pinch fold crease. The implants would be replaced after the tissue expanders have been removed in an outpatient procedure.
Recovery and After Care
Recovery after the tubular breast surgery bears in mind a few things to be kept in mind, which include: Immediately after surgery, you will be taken into the recovery area where the nurse monitors you. As with any other surgery, pain is experienced for which medication is administered to ease the discomfort. Some discoloration, bruising, and swelling are usually expected initially. You will be discharged on the same day to have someone stay with you for the first 24-48 hours, as is common with most surgeries. Most patients will be seen one week later, then every two weeks to monitor the progress until you are fully recovered. Over the ensuing weeks from your tuberous breast correction surgery, the incision lines will continue to heal. It is important that you follow all the instructions given to you. Your scars may occasionally seem to worsen before they start improving. You will also be provided with guidelines on post-operative care meant for the prevention of infection. It is expected that after tubular breast surgery, some swelling, which might last for many weeks, may occur. Your swelling will subside as time goes on, and once your incisions are healed, you will start to see your final results. Taking your vitamins, including any other supplements that are shown to be beneficial to healing, can help a patient limit their recovery process. Full recovery from tubular breast surgery will occur at an individual rate. Your body may take weeks or months to recover entirely- depending on your care during the recovery. Most patients are recommended to walk upon returning home and can usually resume sexual relations in about two weeks. Depending upon the type of surgery performed, for at least two weeks, patients should avoid any activity that can result in a sudden increase in heart rate and blood pressure. Light cycle ergometry may be done after three weeks. Arrange for a friend or family member to be available to help you with activities of daily living for the first couple of days after surgery. It is quite common, while the breasts are healing, to experience mood swings including feeling depressed, weepy, angry, etc. Some women even find they have a lack of concentration among other things. This may be because of the reaction of the body to anesthesia and it might take a few days or a few weeks. So many women complain about shortness of breath, which may also be due to the reaction of the body to anesthesia.
With any surgical operation, there are a host of risks and complications that may arise, though these generally come at a low incidence with tuberous breast reconstruction. The range of complications which may be expected varies from the most common, including swelling and scarring, to the very rare, which may include thrombosis or the loss of sensation in the nipple area. Possible complications, which may arise from any type of surgery, include those of infection; however, instances of post-operative infection following cosmetic breast surgery are very low due in part to standard practices to minimize such risk. Other common complications to breast surgery include bleeding, compromised or slow healing of incisions or wounds, and abnormal scarring. As tuberous breast correction often deals with a breast implant and deep sutures, the additional possible complications related to breast surgery include changes in nipple sensation, asymmetry in the positioning of the implant, capsular contracture, and implant malposition.
In general, the risks and complications associated with tuberous breast reconstruction are similar to those associated with augmentation mammaplasty in general, but there is a higher potential for nipple asymmetry in this subset of patients. The actual complication rates for any given condition listed here are generally very low, and some of the potential complications are very rare. Many risks and complications may be minimized by selecting a Plastic Surgery-certified surgeon who has considerable experience with tuberous breast correction, but a proper understanding of the issues that might impede healing and recovery is also important. Consequently, make sure your complete medical history and what medications or supplements you might be taking are revealed at the time of consultation.r
All plastic surgery should begin with a mutual understanding of patient expectations. Surgical treatment can only be as successful as the goals set at the onset. How tuberous breast surgery works can be quite complex, having clear goals is an important indicator for a realistic and successful outcome. However, expectations should be tempered by an understanding of the variability in tissue healing. Tissue tightness and swelling are necessary in all breast surgery, but particularly so in tuberous breast reconstruction. The breast implants widely used can take their own time to settle. Some implants sit perfectly the very next day after surgery, and some need a gentle massage by the surgeon to shift them to the right position in the early weeks after surgery. Occasionally, a bigger push needs to be made into the pocket at a later stage.
Breast implant position is not just dependent upon the skill of the surgeon; variables include the tissue and anatomical differences in each patient. Anatomical variables not only predict the final result but can also reduce the risk of complications if adequately addressed during surgery. Inadvertent tissue damage during dissection can thwart the best plan. More complications can occur when a patient has co-conditions such as smoking and obesity. Perhaps most important is the variation of human beings from the emotional, psychological, and philosophical perspectives. Not all humans have an identical conception of what looks good and beautiful. Some like upper fullness, some prefer bottom fullness, and some prefer middle fullness. What invokes symmetry and balance in one person might repulse another. What looks good to some can be revolting to others. Consequently, experience shows that individual responses to how tuberous breast surgery works may be unique. Despite the wide gamut of variables that contribute to the outcome, a significant percentage of patients undergoing tuberous breast correction rated their outcome as good or very good. The difference in size observed before surgery is often still visually appreciated after surgery is performed to correct two opposing conditions. Surgeons expect to correct these conditions to come together, but on occasion, they take a little while to complete the journey from their opposing positions. Adherence to the constructed plan can minimize frustration if it were to occur, but a realistic understanding is that the best plan is refined on the day in the operating room when the body’s exact anatomy may finally be exposed for the first time. A little patience regarding a larger implant settling and another undergoing a small elevation can make a crucial difference to the patient’s experiences on both sides of the operating table. Ongoing input from each other can provide the best results.