Home » Stem Cell Therapy

Stem cell therapy is a groundbreaking field in regenerative medicine, offering revolutionary treatments for diseases that were once deemed untreatable. By leveraging the body’s own building blocks—stem cells—this therapy aims to repair, replace, or regenerate damaged cells and tissues, promoting healing from within. With applications spanning from neurological disorders to diabetes, stem cell therapy promises not only a paradigm shift in treating chronic conditions but also a potential for personalized medicine that caters to the unique needs of each patient.
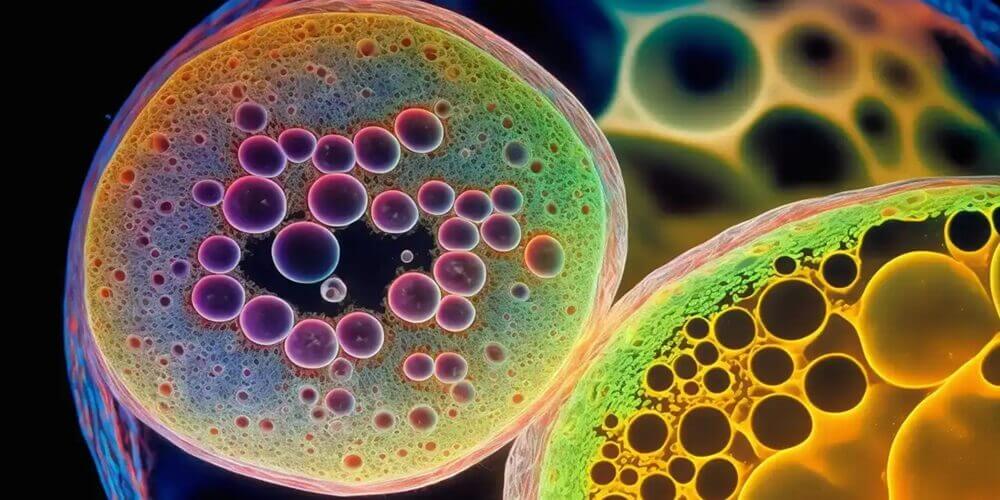
Stem cells are undifferentiated cells with the remarkable ability to develop into various specialized cell types, making them indispensable in growth, development, and tissue repair. There are several types of stem cells, each with unique properties and potential applications:
Derived from early-stage embryos, ESCs are pluripotent, meaning they can differentiate into any cell type in the body. This makes them highly versatile and valuable for research, though their use raises ethical questions regarding the destruction of embryos.
These are multipotent stem cells found in specific tissues like bone marrow, fat, and the brain. ASCs are limited in their differentiation potential, generally producing only cell types associated with their origin tissue. For example, hematopoietic stem cells from bone marrow can produce various blood cells, while mesenchymal stem cells (MSCs) from fat can give rise to bone, cartilage, and muscle tissue.
iPSCs are adult cells that have been genetically reprogrammed to behave like embryonic stem cells. This reprogramming allows them to become pluripotent and differentiate into any cell type, offering similar versatility to ESCs without the ethical implications associated with using embryos.
Stem cell therapy leverages the natural regenerative potential of stem cells, aiming to replace or repair damaged tissues and restore normal function. The therapeutic process generally follows these steps:

Depending on the patient’s condition, stem cells are harvested from a suitable source, which could be autologous (from the patient’s own body) or allogeneic (from a donor). Common sources include bone marrow and adipose (fat) tissue, which are rich in adult stem cells.
In many cases, harvested stem cells are expanded in laboratory conditions to achieve sufficient numbers. During this phase, strict protocols are followed to ensure sterility, cell viability, and genetic stability.
Depending on the targeted tissue, stem cells may undergo differentiation in vitro (in the lab) to pre-specialize them into the desired cell type before administration.
Stem cells are delivered directly to the target area through injection or infusion. For conditions affecting localized tissues, such as cartilage damage, injection directly into the joint may be effective. For systemic diseases, stem cells may be delivered via intravenous (IV) infusion.
After administration, the patient’s progress is monitored to assess the therapy’s effectiveness and to check for potential adverse reactions. Follow-up includes imaging studies, blood tests, and regular consultations to evaluate improvements in symptoms and overall health.
The potential applications of stem cell therapy extend across numerous fields of medicine. Below are some key areas where stem cell therapy is actively researched and utilized:

Stem cell therapy offers a range of potential benefits that differentiate it from conventional medical treatments:
While stem cell therapy holds immense promise, it is not without challenges and ethical concerns.
The future of stem cell therapy is promising, with ongoing research aiming to expand its applications and improve treatment efficacy. Emerging technologies and techniques are shaping the next frontier of stem cell therapy:
CRISPR gene editing technology is increasingly being integrated into stem cell research. By editing the genes of stem cells before transplantation, scientists hope to treat genetic disorders at their source.
3D bioprinting is a cutting-edge field that uses stem cells to create tissue structures layer by layer. This technique could eventually enable the production of organs for transplantation, addressing the shortage of donor organs.
Stem cell therapy represents one of the most exciting advancements in modern medicine. Its ability to regenerate damaged tissues, treat chronic diseases, and potentially revolutionize personalized medicine holds immense potential for the future. However, continued research, ethical scrutiny, and regulatory oversight are crucial to ensuring that stem cell therapies become a safe and accessible option for all.
Hello!