Home » Will There Be Any Scars After Breast Reduction Surgery?

Scars are the most commonly discussed issues by patients considering surgical procedures. This is well-founded as the emotional sequelae of scarring can be as difficult for the patient to cope with as the physical disfigurement. Unattractive scars are not uncommon after breast reduction in Turkey, though many are inconspicuous. It is necessary to understand the basics of scar aesthetics, including the predominant types of scars and potential quality identifiers such as color, retraction, orientation, width, or elevation. With a greater understanding and the development of techniques to ensure the best outcomes, patients can be counseled more satisfactorily in the pre-operative period, confounding the association with patient dissatisfaction. Expectation has been strongly linked to patient satisfaction after cosmetic surgery, with morphologic changes, scarring, and complications all featuring as the most common reasons for dissatisfaction overall.
Several factors related to wound healing and therefore scarring make summary statements less than straightforward. For example, the genetic background of the patient is of some relevance. There is a strong genetic control of the physical and functional properties of collagen. It has been demonstrated that there are measurable differences in scars after cesarean section taken from identical twins in 25 of 35 physically measured variables of healing examined. The cellular rate of response may also determine a scar’s final quality. Cases with low cellularity may heal slowly and with a diminished collagen deposition rate. The blood supply, size, and geographic nature of the defect may limit wound closure modalities available to the treating surgeon and are factors which, like the patient’s genetic background, are ultimately beyond the surgeon’s control. Given these limiting factors, however, many strategies can and have been utilized such that resultant breast surgery scar heal to be minimally noticeable. In this paper, we consider these strategies.
Given the multifactorial nature of wound healing, it is highly probable that scarring is influenced by multiple variables. Individual differences such as skin type, inherited predisposition, and age affect the look and behavior of each breast surgery scar. Wound tension, created by the surgical technique itself as well as the size and location of the resection, could potentially improve adhesion and reducing scar visibility in the dermal suture. Dermabrasion is practiced for peeling the stratum corneum of the skin, promoting a more asthenic, irregular, and attractive scar. Exposure to the sun post-operatively seems to affect the final quality of the scar as well, posing a very delicate problem of management especially with patients from warm climates.
The presence of factors such as diabetes and hypertension, steroid-dependent diseases, certain malignancies, and old age can reduce the metabolic energy of the scar by as much as 25% as can smoking. A good nutritional state and immune system as well as adequate perfusion diminish the risks of wound complications. Finally, ethnic factors have to be considered, since scarring in darker biotypes seems to be of better quality than in lighter ones. In general, dermatosurgery adheres to practices that appear to create the least scarring, necessitating the smallest incisions, preferably along relaxed skin tension lines, with minimal wounding or trauma made carefully and precisely. All of the above techniques have been used quite extensively and systematically among numerous operations involving different anatomical sites and have proven to be safe and reliable; practices of the art and, according to some, a true, delicate and complex surgical philosophy. In specific anatomical sites, practitioners have reported a marked improvement in the final quality of the scar. On the other hand, procedures such as undermining have been reported to potentially compromise objective results by undermining tissue perfusion, thus bringing about ischemic complications. Since a significant part of the alterations of local hemodynamics or the mechanisms of wound healing produced manifest changes in local temperature and, consequently, in the cutaneous thermogram, thermography may become helpful in judging the short- and long-term outcome of these practices. These are of practical relevance for both patient and practitioner in dermatosurgery, especially when aesthetic results are essential to the patient. The final decision as to the location and shape of the scar has to be made on an individual basis for each patient and on the basis of each surgeon’s skills. The optimizing of personalization in the dermatosurgical treatment plan will without doubt limit expectations as far as a less unsightly scar is concerned since good and/or excellent results are part of an often idealistic aesthetic concept.

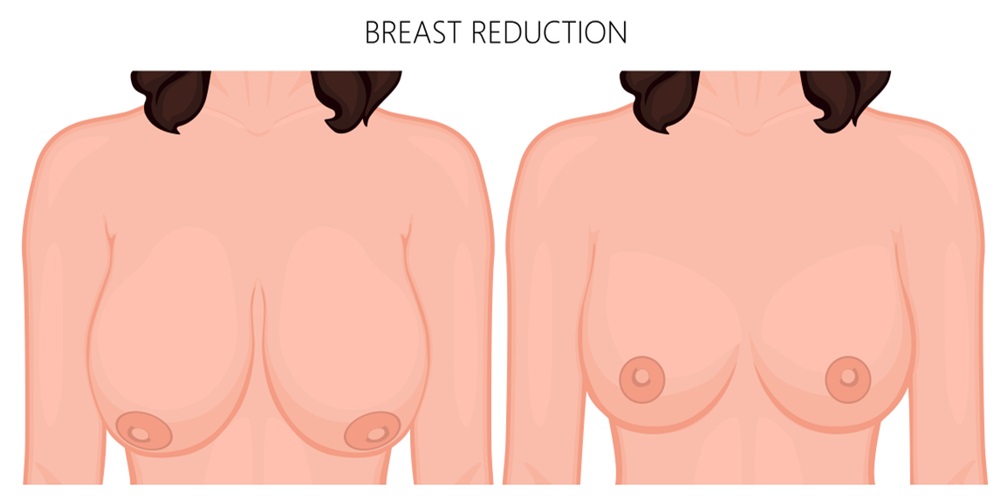
Techniques and innovations for breast surgery scar reduction. In cases of breast reduction surgery, the goal of minimal incision plastic surgery is to create a new breast with the appropriate size, position, and shape, taking into account each patient’s individual breast characteristics. However, in order to achieve the optimal aesthetic outcome, the incision is planned and buried in regions that heal most quickly, such as at the inframammary groove of the site of the concentration of the main breast reduction in Turkey tissues. The additional use of hand-assisted laparoscopic equipment with a miniature camera and long forceps makes it possible to limit the width of the required incisions and minimize the occurrence of scars. Some patients have the ability to heal rapidly from scars, resulting in reducing scar visibility width and color. To optimize aesthetic results, evaluation is performed by a board-certified dermatology specialist to plan postoperative follow-up regimens up to several years after surgery. Development of a new-generation high-precision erbium-doped yttrium aluminum garnet laser is also being considered in curative treatment methods for scars following breast reduction surgery. New medical devices attach to the ears and can be set to a specified wear frequency, allow treatment remotely according to the treatment timing, and produce an adequate effect in patients’ daily lives. In addition, many new medical devices have been developed, studied, and presented to treat breast surgery scar. Postoperative follow-up management conducted by surgical and dermatology departments may lead to additional improvements in reducing scar visibility width at the final assessment. More research is being conducted, including prospective methods, to investigate the cosmetic result after breast reduction Turkey and the formation of postoperative scars. By continuing to discuss and disseminate information, plastic surgeons will be able to accumulate more knowledge and improve their techniques for the prevention of postoperative scars at reduced sites using diverse approaches and useful methods.

Proper post-operative care of the reduction mammoplasty scar is of critical importance. While there are many products and contraptions intended to assist in reducing scar visibility, there is little evidence to support one intervention over another. This can lead to confusion and skepticism surrounding the true efficacy of these products and procedures. Due to the lack of documented follow-up, patients may lose interest and not adhere to the regimens advised to them. It is critical that there is thorough patient education to promote self-care and adherence to the care agenda. Encouragement should be provided to patients to participate actively in the reducing scar visibility. This can encompass several methods that should not replace the necessity of the patient attending a scheduled appointment.
Topical agents such as silicone sheets have been used for years to manage hypertrophic scars and keloids by healing the scar from the outside in. It is believed that silicone sheets provide moisture, create pressure over the wound, and assist in maintaining a hydrated wound while it heals. Scar massage has been practiced for many years and is based on the principle that the action of massaging a surgical scar can result in changes in the mechanical properties of the skin and soft tissues. This disruption in scar tissue layering may soften and distribute the scar throughout the soft tissues. Recommendations for the most beneficial time to institute massage range from shortly post-operatively up to 6 weeks after surgery. A recent trial, involving the use of massage and moisturizing with patients post breast reduction in Turkey surgery, found that the massaged scars improved in pliability and vascularity as opposed to the moisturized scars. The same trial found that the scars of the massaged patients were preferred by both the patients and the clinical assessors throughout the follow-up period. It was also found in a trial of participants that those people who undertook self-massage of their moisturizing topical had improved scars over the control group months post-operatively. The time that the patients should invest in the massage regimen is varied in the literature. Typically, a recommendation of 15 to 20 minutes of massage to the area is needed. The massage should be gentle but firm, and the patient should be made aware of when to cease the massage if they experience discomfort.
Hello!