Home » What to Expect During Breast Reduction Surgery?

Breast reduction procedure, or mammoplasty, also known as reduction mammoplasty, is a plastic surgery procedure that involves reducing the size of the mammary glands. This life-altering operation is always done with the consent of the patient. While most individuals opt for regular breast reduction procedure, cosmetic surgeons may recommend liposuction in some cases. The methods are somewhat similar, but this report will focus only on surgery process breast reduction and the associated concerns, as it is important.
The main side effect of surgery process breast reduction for most people is the recovery period, which typically lasts around 4-6 weeks. During this time, a bed rest program is required, and it is important to allocate time for relaxation whenever possible. During breast reduction procedure, fat, glandular tissues, and skin cells are removed from the breasts. Women with breast hypertrophy (abnormal growth after the maturation process) or hysteroptosis hypertrophy (normal growth after the maturation process of overlarge organs) are the two groups that most frequently undergo breast reduction procedure. The main purpose of the surgery is to balance the size of the breasts and make them proportionate. The cosmetic surgeon strategically cuts pink and cauliflower tracts, which must be known in advance for the success of the procedure. In order to minimize post-procedure complications, in-and-out incisions are made for the simplest surgery process breast reduction.
Although surgery process breast reduction can provide relief from a wide range of physical problems, many patients have psychological concerns regarding their postoperative appearance. This caution would appear to be well placed, as there is evidence that breast reduction can have an adverse effect on women’s body images, especially in women who continue to perceive their breasts as abnormally large after surgery. Further, Skinner and Gelsomino suggest that surgeons should be wary of operating on women with body image “overconcern”, who are generally dissatisfied with their general appearance and often undergo multiple plastic surgery procedures. A better understanding of presurgery attitudes and expectations may aid in identifying those patients who are potential candidates for psychological intervention at the time of surgery or during the preoperative consent process.
Most studies that consider the psychological impact of breast reduction have investigated the effect of breast hypertrophy on psychological well-being and quality of life using generic or breast-specific outcome measures, or surgical satisfaction questionnaires. Such studies have noted that women with macromastia often experience depression and have a poor body image, with a significant subgroup upper cervical cost, as a high-impact study has recently shown. The use of validated objective measures rather than subjective judgments presents as an advantage to this study. In addition, “ideal breast size” was not correlated with satisfaction with the result, despite some patients might be expected to have their breasts reduced to ideal size.
Breast reduction procedure is generally very effective and can have a dramatic impact on a young woman’s quality of life. People need to know what to expect breast reduction in most cases. Most women are extremely satisfied after the procedure, and most men receive immediate relief from their symptoms. The risks of the procedure are relatively low, though not zero. In general, there are three types of complications. The most common is a small risk of wound healing problems during the recovery process. These problems are usually quite minor and are usually not recognizable past the first two months after the surgery. There is a small risk of an adverse reaction to anesthesia and blood clots in the legs that can result in a clot going to the lung. Such serious events are extremely rare – to happen in only about 1 per 2,000 to 3,000 patients. Finally, there are certain changes that occur as part of the body’s natural wound healing process (scar). Most women continue to have improvements in the breast shape as their scars mature over the first two years after surgery.
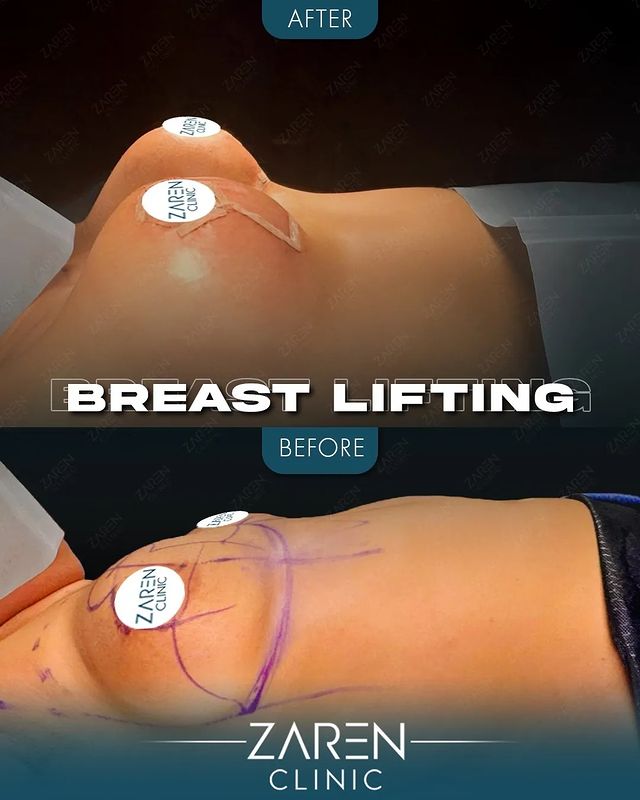
There is no cure for stretch marks, and though they do not spread or cause any serious medical problems, they are permanent for life. Finally, while this is a vastly understudied area, breast reduction may result in a small but unlikely loss of nipple sensation. Breast reduction surgery, also known as the reduction mammaplasty, is a commonly performed procedure that is known to reduce the size of large, heavy breasts in proportion to the rest of the body. While the technique will vary by surgeon and patient, key steps include altering nipple position to be more aesthetically pleasing, lifting the breast tissue to be less saggy and more tight, and removing part of the skin and breast tissue so that the breast is smaller.
For many with oversized breasts, the potential medical benefits of undergoing surgery process breast reduction are clear-cut. And despite the prospective benefits, many may remain concerned about the immediate and “upfront” costs and if their insurance will cover the expense any better. While tailored for each patient and their desired modifications, breast reduction procedure certainly is not an inexpensive undertaking, causing many to shoulder a heavy financial burden in the form of direct, out-of-pocket expenses.
For example, the average fees listed above merely begin to approach the scope of what may be charged for a breast reduction and would not only require a consultation to discuss a patient’s requests, chances for candidacy, surgical plan of action, starting a new drug energy enhancer, as well as 6-months of using a skin-expanding supplement (to achieve optimal results) prior to the procedure (for no extra cost—and would have great utility for abdomen or buttocks enlargement, too!); but also present additional fees for implants, anesthesia, disposable surgical supplies, expenses related to medical testing (x-rays, urine and blood work, etc.), operative facility and recovery room costs, compression garments, and follow-up visits. Individually and collectively, it is little wonder how crossing this “financial threshold” would assume significant concern and apprehension for many candidates who would greatly benefit from surgery process breast reduction—leaving some entirely unable to “comfortably” afford it. In other cases, some candidates might be fortunate enough to navigate excessively confusing insurance policies and find that some carriers will help to cover or defray part of the cost for their insured to have their breasts reduced.
Overall, breast reduction procedure helps to alleviate many of the social and psychological ailments that disproportionately burden adolescent and adult women with overly large and ptotic breasts. However, as can be seen from the case reports, it does not come without significant burden to the patient for the surgery, postoperative care, and complications. In this regard, accurate assessment and management are of great importance. Future studies may also focus on the satisfaction of outcome for surgery process breast reduction as well as patient’s quality of life after treatment.
On the front, there are three main players who want to know that their effectiveness, safety and health outcomes for patients seeking breast reduction procedure is crucial. In this case, patients want to know what the outcome of the surgery is, including, among potential complications. If the patient chooses BR as a way of raising their breast size, they should be aware of the complications and possible complications. Complications ranged from 2.2% to 4.8%. Izziye-Ihara et al any queries reported were addressed. Simons et al have shown that edge abscesses are the most common of Baumann complications.