Obesity is the most vulnerable problem in our era. And, many people suffer from it. Nevertheless, there is many treatment types of this diseases. Medical treatment for weight loss is generally insufficient. Surgery has become the mainstay of treatment for morbid obesity. For this purpose, some surgical techniques have been used in the last 60 years. Roux-en-Y gastric bypass, sleeve gastrectomy, adjustable gastric band, and biliopancreatic diversion are the most commonly performed current surgical procedures.
All of these procedures can be performed laparoscopically. Reduced food intake and early satiety due to a decrease in stomach volume by surgery and impaired absorption due to bypass lead to significant weight loss. In this article, we explore these treatment. First of all, we give information about obesity. After that, we examine which surgical techniques for obesity are available and what are these.
What is Obesity?
Mortality of Obesity has become an epidemic problem in recent years. Also, it is second in preventable diseases caused by mortality after smoking. In Table 1, you can see changing people who have obesity the recent decade.
Table 1: Chancing Obesity Recent Decade
| Year | Obezite Rate (%) |
| 2010 | %12.0 |
| 2011 | %12.2 |
| 2012 | %12.4 |
| 2013 | %12.6 |
| 2014 | %12.8 |
| 2015 | %13.1 |
| 2016 | %13.3 |
| 2017 | %13.5 |
| 2018 | %13.7 |
| 2019 | %13.9 |
| 2020 | %14.1 |
| 2021 | %14.3 |
When we look at table 1, we can easily see an increase in obesity. From poor eating habits to sedentary life-style, many reasons play a role in obesity. So, how to calculate obesity?
Calculating Obesity
How to calculate obesity? The answer to this question is quite easy. Below, you can see calculating obesity. You can easily apply this formula yourself.,
Table 2 Calculating Obesity
| BMI (kg/m²) | Classification of Obesity |
| < 18.5 | Thing |
| 18.5-24.9 | Normal |
| 25.0-29.9 | High weight |
| 30.0-34.9 | 1. degree Obesity |
| 35.0-39.9 | 2. degree Obesity |
| ≥ 40.0 | 3. degree Obesity |
For example, if one have 85 kg weight and 1.75 mt leghth, Obesity calculation is below;
BMI = weight (kg) / height squared (m²) BMI = 85 / (1.75 x 1.75) = 27.8
According to this calculation, he/she is in the category of high weight.
The Metabolic Effect of Obesity
Due to increase BMI, some diseases defined as “Metabolic Syndromes” is frequent. In this case, the cardiovascular risk rises three times. As depending on the metabolic effect of obesity, many diseases occur. For example, these diseases are below, respectively;
- Osteoarthritis
- Type 1 Diabet
- Gastro-oesophageal reflux disease (GORD)
- Congenital central hypoventilation syndrome (CCHS)
- Hypertension
- Kolelitiazis
- Some types of cancer
- Migraine type headache
- Increased Mortality risk
Also, %90 of patients can have Non-alcoholic fatty liver disease (NAFLD) and steatohepatitis is in %25 of them. With weight loss, many patients recover. In addition, the life expectancy of men patients aged 21, having morbid obesity, is lower than 12 years normal person. In women, this time is nine years.
Surgical Treatments Options in Morbid Obesity
Obesity is not only physical disease, it also occur many psychological diseases. Therefore, fighting against obesity is important. Although weight loss is achieved with non-surgical methods, 66% of patients become obese again in a short period of 24 months. The patient’s compliance with the diet during medical treatment may form an opinion about the patient’s compliance after surgical treatment. The surgical option has come to the forefront in the treatment of morbid obesity as it causes early deaths due to comorbidities and has become epidemic.
Surgical treatment of morbid obesity is called bariatric surgery. Bariatric surgery provides long-term permanent weight loss, prevents many comorbidities and increases survival by reducing the metabolic effects of obesity. Sustainable weight loss is achieved only with bariatric surgery. Bariatric surgery provides more than 50% reduction in excess weight.
Surgical treatment is a part of a bariatric programme with long-term follow-up and evaluations. In the treatment of morbid obesity, surgery is a pillar of a multidisciplinary approach. The results of surgical treatment are better in patients with good motivation, educated patients who participate in multidisciplinary evaluations, and patients in whom medical treatment has failed. Substance abuse is a definite contraindication for surgery. The requirements for bariatric surgery were set out in the consensus decisions of the US National Institute of Health (NIH) in 1991.
The most common bariatric surgical procedures
Restrictive (restrictive)
- Laparoscopic adjustable gastric band (LAGB)
- Sleeve gastrectomy (SG)
- Vertical band gastroplasty (VBG)
Absorption disruptor
- Biliopancreatic diversion (BPD)
- Jejunoileal bypass (JIB)
Combined restrictive and malabsorptive
- Roux-en-Y gastric bypass (RYGB)
- Duodenal switch (DS) with BPD
The mechanisms of action of bariatric surgical procedures are the result of complex interactions of malabsorption and gastric resection, as well as hormonal and neural signals affecting hunger and satiety. In a meta-analysis, Buchwald et al. reported the rates of improvement in diabetes with bariatric surgery as 56.7%, 79.7%, 80.3% and 95.1% for adjustable gastric band (AGB), Roux-en-Y gastric bypass (RYGB) and bilio-pancreatic diversion-duodenal switch (BPD-DS), respectively. Complete diabetes remission was observed in 78% of patients. Lipid profile improves in 70% of patients after bariatric surgery. Total cholesterol, LDL and triglycerides decreased while no significant change in HDL was reported. Mortality rates in bariatric surgery procedures are equal to those of minor intra-abdominal operations such as laparoscopic cholecystectomy (0.3-0.6%).
Bariatric surgery dates back to the 1950s when absorption-reducing operations were performed for the treatment of severe hyperlipidemia syndromes. All bariatric surgical procedures are mostly performed laparoscopically. The most commonly performed bariatric surgical procedures are RYGB, SG and AGB.
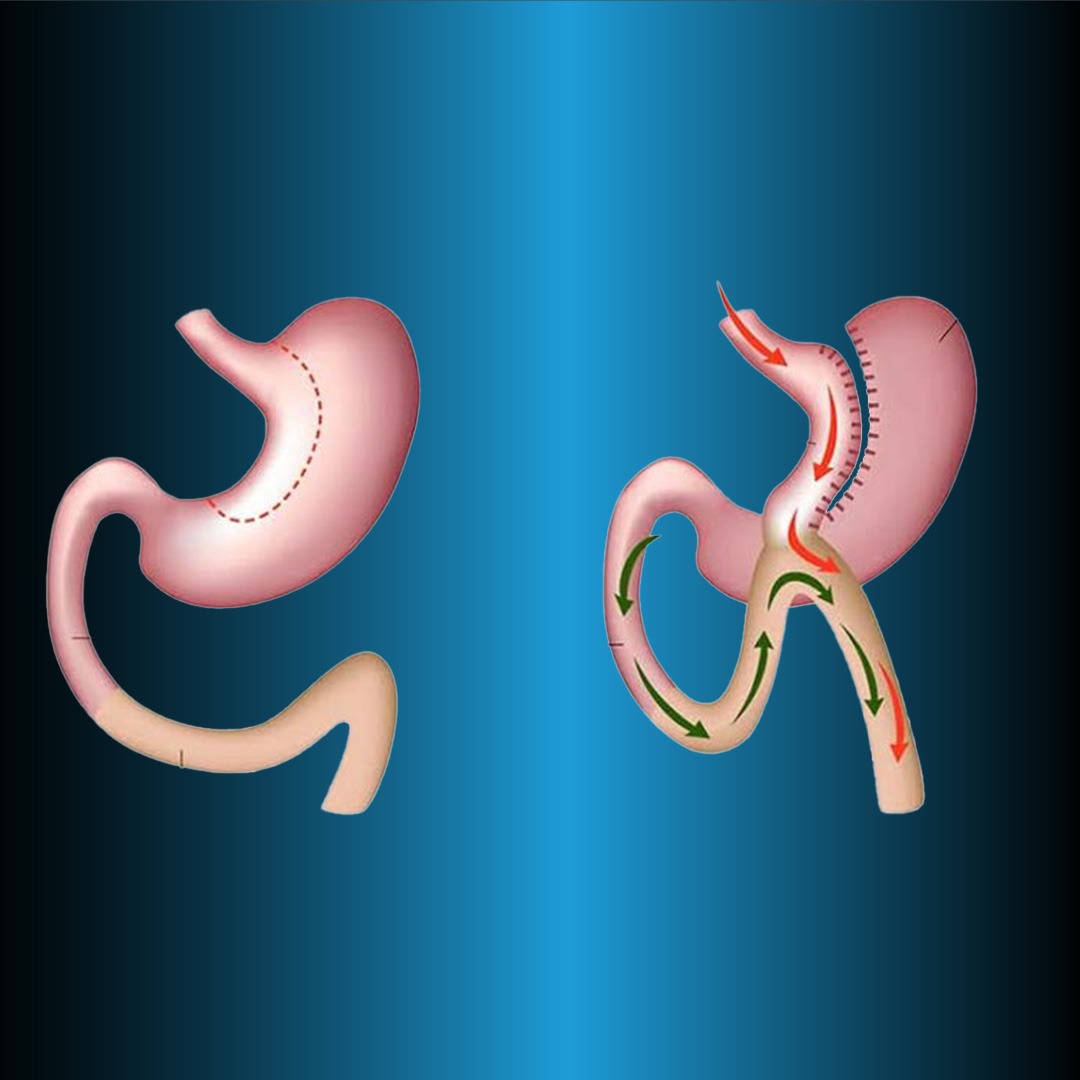
Laparoscopic Roux-en-Y Gastric Bypass (LRYGB)
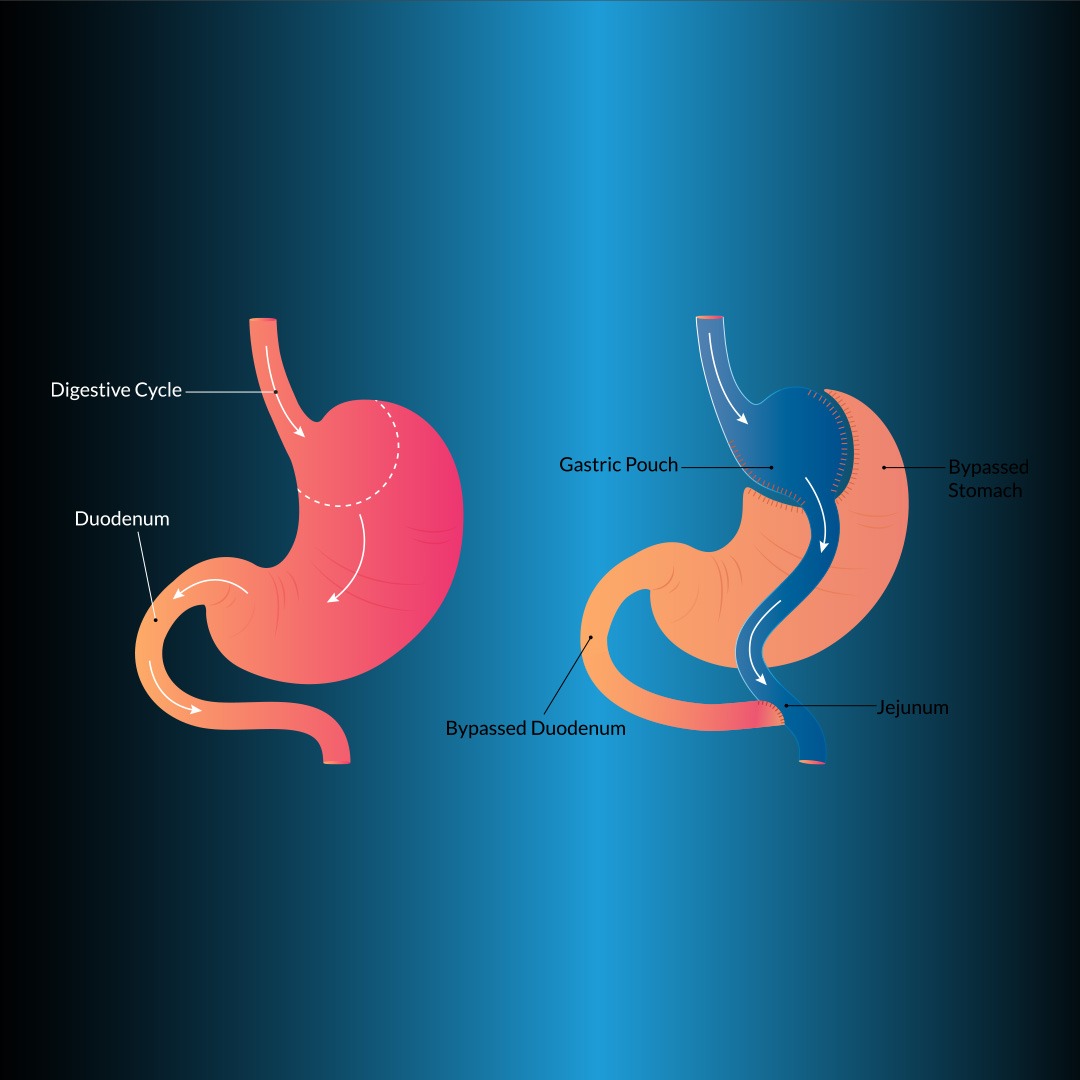
It is the most commonly applied volume-restricting (restrictive) method. LRYGB is considered to be the gold standard in the surgical treatment of morbid obesity because it provides long-term permanent weight loss and has acceptable morbidity and mortality. The gastric bypass method in bariatric surgery was first introduced by Edward E. Mason. In this method, 90% of the stomach volume is reduced and malabsorption is achieved by bypassing the duodenum.
The main procedure in this technique is to create a small volume (<20 mL) gastric pouch completely separate from the stomach proximally (Figure 1). For gastrojejunostomy, the Roux leg can be pulled up anterior to the colon and stomach, anterior to the colon and posterior to the stomach, or posterior to the colon and stomach. Transoral circular stapler, linear stapler, manual suturing, or transgastric circular stapler techniques can be used for gastrojejunostomy. The length of the biliopancreatic leg is 50 cm distal to the ligament of Treitz and the length of the Roux’s leg is 100-150 cm.
How to perform it?
The stomach is cut with a linear stapler (60 mm in length and 3.8 mm in thickness) 3-5 cm distal to the oesophagogastric junction perpendicular to the small curvature and then the pouch is formed by completing the cutting process towards the angle of sensation. Postoperative fluid support and adequate urine output are very important. Postoperative follow-up at the 3rd week, 3rd month, 6th month, and 1st year should focus on the results and nutritional deficiency.
These patients lose 60-80% of their excess weight within 1 year after the operation. Accordingly, co-morbid diseases are also significantly improved. Morta¬lity is <1% and morbidity is 15%. Postoperative complications such as leakage (1-2%), stenosis (1-19%), small bowel obstruction-internal hernia (7%), and a marginal ulcer (3-15%) may occur. Since it may lead to long segmental necrosis, urgent surgical intervention is required when an intestinal obstruction is considered. RTGB is more effective than LAGB, especially in the management of type 2 DM and gastro-oesophageal recurrent disease (GERD) symptoms.
Sleeve Gastrectomy (Vertical Gastrectomy)
Sleeve gastrectomy (SG) was first introduced as the restrictive component of DS surgery. In patients who are super obese and in whom DS is risky, sufficient weight loss is achieved in the early period with SG alone. This method has entered practical application as a risk-reducing method in high-risk patients who cannot tolerate long-term procedures. Laparoscopic sleeve gastrectomy (LSG) has become a safe and effective primary bariatric surgical procedure with high popularity for surgeons and patients and an increasing frequency of application. LSG accounts for 5% of all bariatric surgical procedures and the number of patients is increasing rapidly.
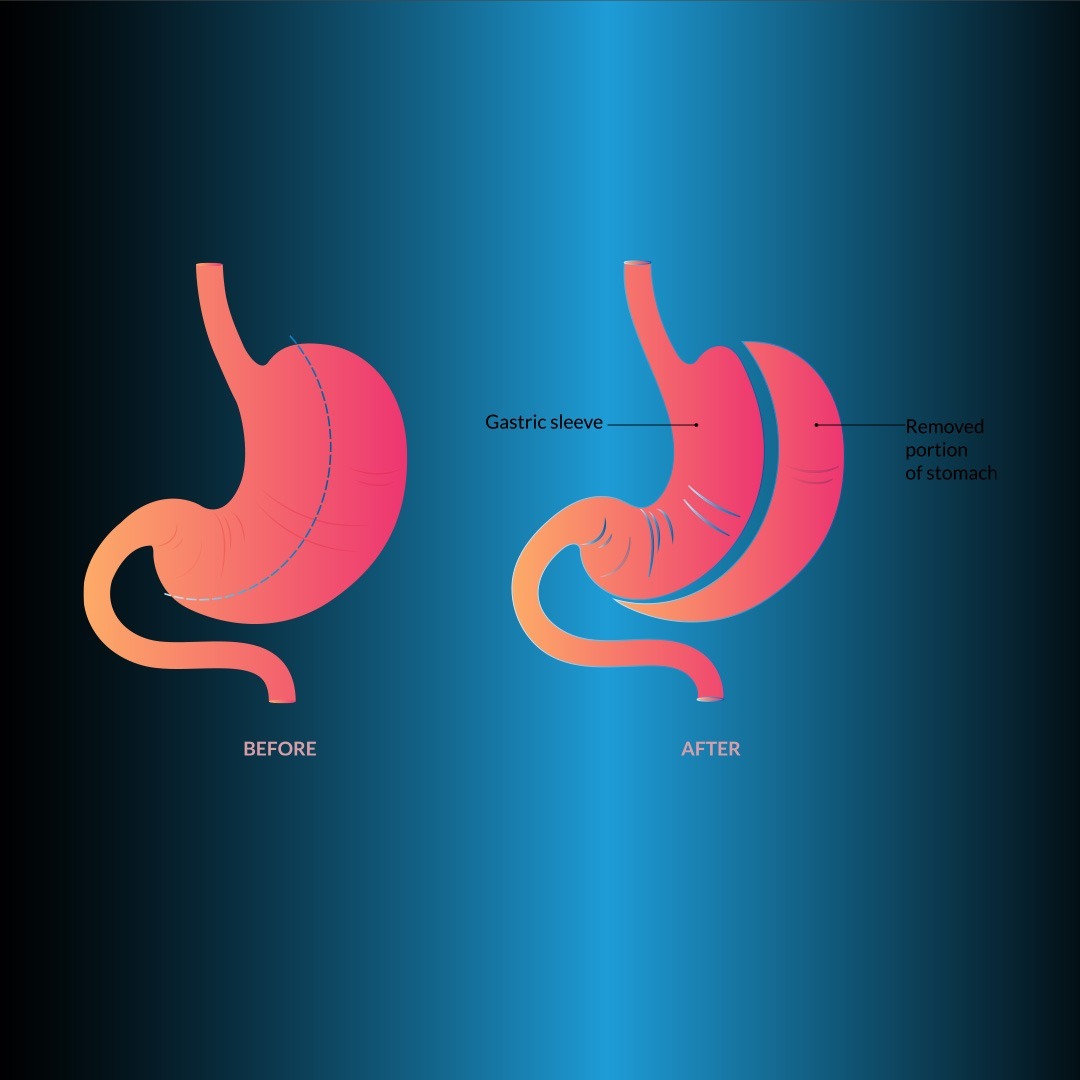
With this method, a narrow tubular stomach is created (Figure 2). After the greater curvature is freed 2-3 cm proximal to the pylorus up to the His angle, gastric resection is performed. Tissue staples of 4.5 mm (thick) in the antrum and 3.8 mm (medium) in the other gastric parts are used. In order to leave a large fundus pouch, posterior dissection should be done very well so that the sensory angle is visible.
If the lateral traction of the stomach is not good, a spiral shaped resection line may form. To reduce the risk of leakage, 1 cm of gastric serosa should be seen on the left edge of the stapler cartridge before firing the last stapler. After resection, leakage and bleeding in the stapler line is checked with an endoscope.
How to perform it?
Omentum is sutured to the suture line to create a potential barrier in case of a possible leak. By suturing the omentum or gastrocolic fat, the sleeve tube is fixed, and bending of the stomach through the incisura angularis is prevented. LSG is thought to have a slimming effect by being restrictive, decreasing ghrelin, and increasing PYY and GLP-1 hormones with the rapid passage of food to the distal. LSG is preferred in super obese and patients with BMI <50 kg/m2 who desire this method. In the systemic examination of 2500 patients (mean BMI: 51.2 kg/m2) in whom this method was applied, mean excess weight loss was 55%, the complication rate was 8%, and the mortality rate was 0.19%.
While diabetes remission was reported to be 66.2% in LSG, 15% of patients may require a new bariatric intervention (22,23). LSG has become a frequently preferred method alone or in combination with other methods in the treatment of morbid obesity. The most important complication is leakage (2%), which is frequently seen near the His angle. The causes of leakage include placement of the last stapler line close to the esophagus, stenosis of the incisura angulars, and bending of the tubular stomach. GERD occurs in 26% of patients after LSG. In the case of refractory GERD, the revision surgery should be performed.
Laparoscopic Adjustable Gastric Band (LAGB)
FDA approval of LAGB in the USA has been available since 2001. This method achieves weight loss by reducing food intake with its completely restrictive effect. A 25-30 cm reservoir is created proximally by wrapping an inflatable silicone band around the stomach 3 cm below the oesophagogastric junction. At the other end of the band is a port placed under the skin (Figure 3). The caliber of the gastric opening can be changed by filling and emptying the silicone band with serum under fluoroscopic guidance. The band is initially placed completely deflated. Since band prolapse and erosion are less common, the pars flaccida technique has become standardized.
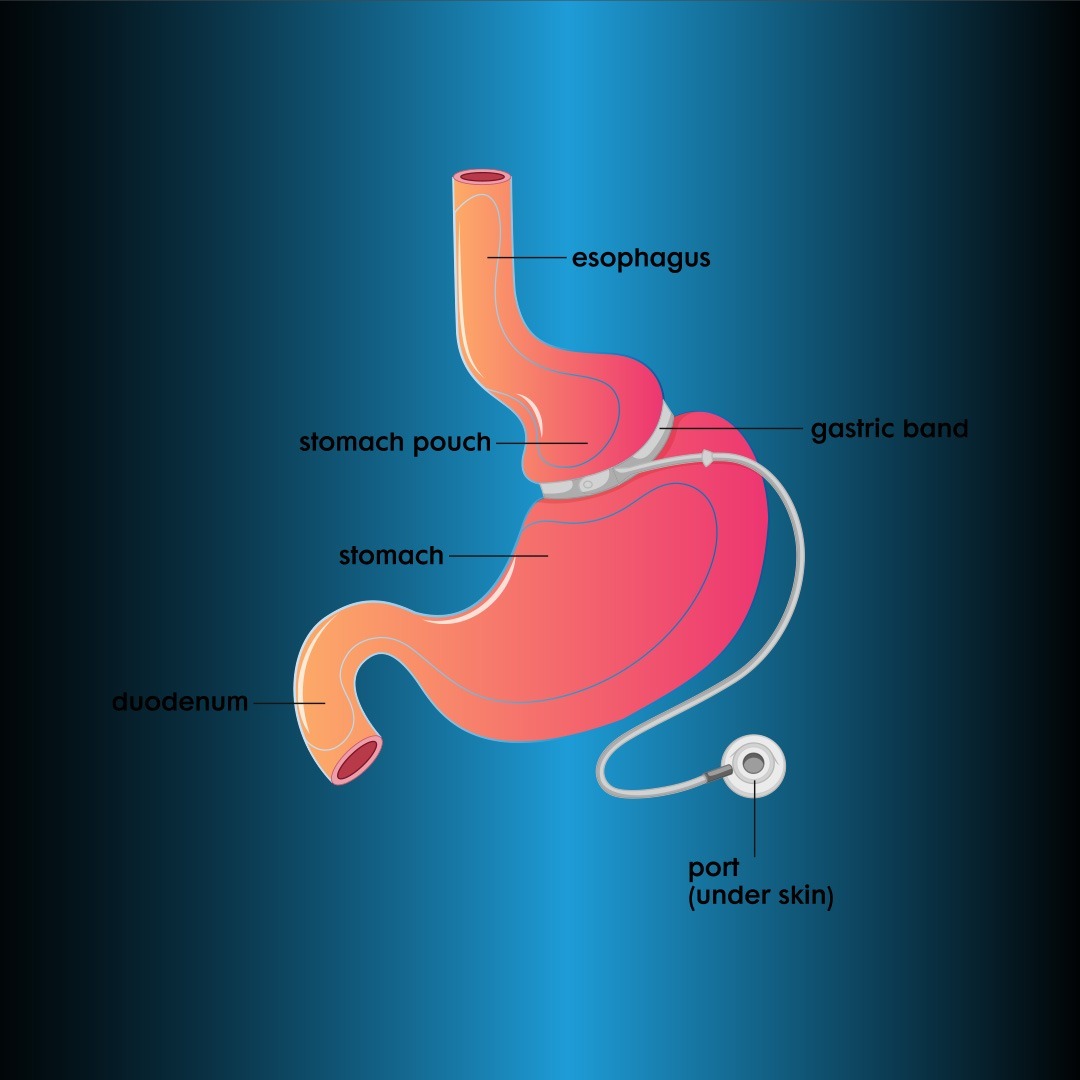
Since the LAGB method requires frequent follow-up, it should be applied to patients living in close areas with easy access to the hospital. Patients are only recommended multivitamins after surgery. Adjustment of the band is as important as surgery. In this method, a loss of 0.5 kg per week is ideal. Patients lose 58-60% of their excess weight in 7-8 years after surgery. Complications and mortality rates are less compared to malabsorptive techniques. Prolapse (3%), slippage (<3%), band erosion (1-2%), and port and tube complications (5%) may occur. Although the high reoperation rate is the most important disadvantage, this technique is still popular in the USA.
Biliopankreatik Diversion and Duodenal Switch (BPD-DS)
The biliopancreatic diversion and duodenal switch (BPD-DS) procedure is often referred to as duodenal switch (DS) surgery. This technique is a modification of the original biliopancreatic diversion described by Scapinaro (28) in 1979. The three main components of this technique are gastric sleeve formation with pylorus preservation, distal ileoileal anastomosis, and proximal duodenoileal anastomosis. As in RYGB, three intestinal legs are formed in this method. Food passes through one leg (Roux’s leg), digestive fluids (bile) through one leg (biliopancreatic leg), and food and digestive fluids through the common leg.
In the BPD-DS operation, the small curvature of the stomach is removed and the pylorus is preserved, while in Scapinaro’s original operation. Also, the pylorus is removed with distal gastric resection. In both techniques, the gastric pouch is 250 mL and malabsorption is created by Roux-en-Y reconstruction of the distal intestines.
The main leg is prepared 50-100 cm, the alimentary leg 250 cm, and the biliopancreatic leg is joined 100 cm proximally from the ileocecal valve. Since the pylorus is protected in the BPD-DS technique, complications such as circle, dumping, and marginal ulcer are less common. At the same time, this method can be performed in stages to reduce complications. If sufficient weight loss cannot be achieved with LSG, BPD is performed after 6-12 months. Glucose control with BPD-DS surgery is better than medical treatment in severely obese patients with type 2 diabetes.
Effect of BPD-DS
Although the technique is well described and effective weight loss is achieved, the BPD-DS procedure is not commonly performed. While SG provides early weight loss, impaired fat absorption is responsible for long-term weight loss. At the same time, decreased ghrelin and increased peptide-YY also increase weight loss in BPD-DS. Therefore, hormonal changes, as well as mechanical changes, may be responsible for weight loss in this technique.
Operative mortality is around 1%. Postoperative complications are similar to RYGB. Patients require high doses of vitamin and mineral supplementation postoperatively. Improvement in comorbidities after BPD-DS is excellent. 92% of diabetics and 90% of sleep apnoea patients recover completely, while 80% of asthmatics reduce their medication dose.
When BPD-DS was compared with RYGB in superobese patients, the improvement rates were in favor of BPD-DS in type II diabetes (100% and 60%), hypertension (68.0% and 38.6%), and dyslipidaemia (72.0% and 26.3%), while the improvement of GERD was higher in RYGB (76.9% and 48.57%). Vitamin supplementation to prevent postoperative malnutrition requires close follow-up.
This method can be recommended for superobese, those who cannot exercise and diet after restrictive methods, and those who need revision surgery after previous failed methods. This method should not be applied to those who cannot be closely monitored, whose income is not suitable for vita¬min support, and those with previous calcium, iron, vitamin, and mineral deficiency. Furthermore, vertical band gastroplasty (VBG), laparoscopic mini gastric bypass (LMGB), and laparoscopic large curvature plication (LBKP) are less common methods in morbid obesity surgery.
CONCLUSION
Bariatric surgery is considered to be the most effective method for long-term weight loss in morbidly obese patients. Bariatric surgery provides an improvement in metabolic disorders such as type 2 diabetes, dyslipidemia, and hypertension. These favorable effects occur as a result of endocrine changes as well as weight loss. As a result, the mortality rate decreases in patients. All these favorable effects can be further enhanced by careful patient selection. Currently, four main bariatric procedures (LRYGB, LSG, LAGB, and BPD-DS) are performed safely and effectively in a cost-effective and minimally invasive manner. For more information about bariatric surgery in Turkey, you can contact Zaren Health.